“Every shift, my colleagues and I are identifying issues to look into and finding appropriate ways to address these. There are things that can be done. Some are easier than others. We’ve also identified systemic areas that will require more work.” - Dr. Ka Wai Cheung, ER Physician
- ED physician and Steering Committee Co-chairs: Dr Zafrina Poonja and Dr Ka Wai Cheung
- Department Heads: Dr Heather Lindsay and Dr Chris Lee
At Vancouver General Hospital, physicians are zeroing in on wellness and burnout challenges by addressing issues and solutions at the department level, starting in the Emergency Department.
Our story: takeaways

Managing a hospital-wide issue
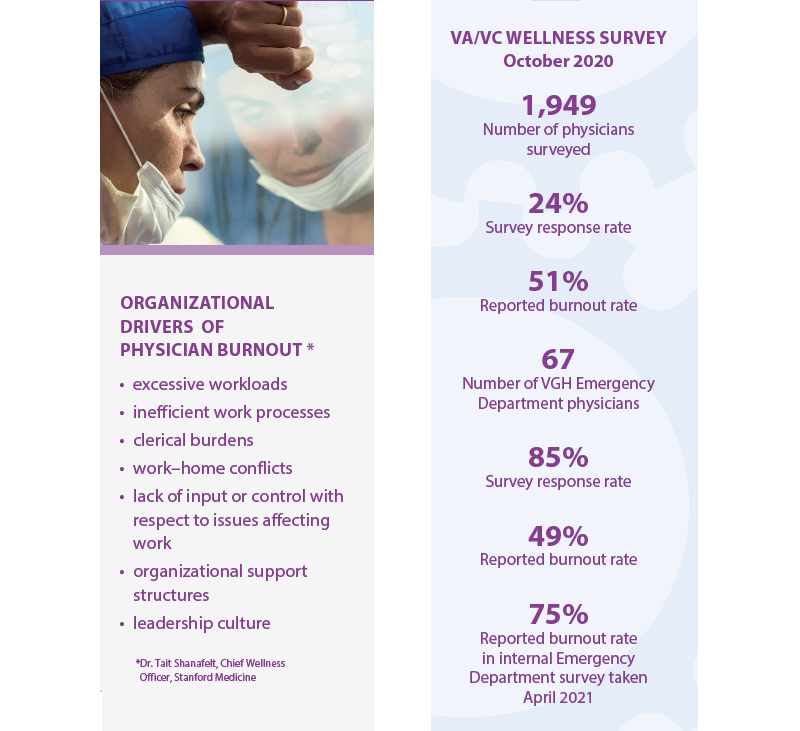
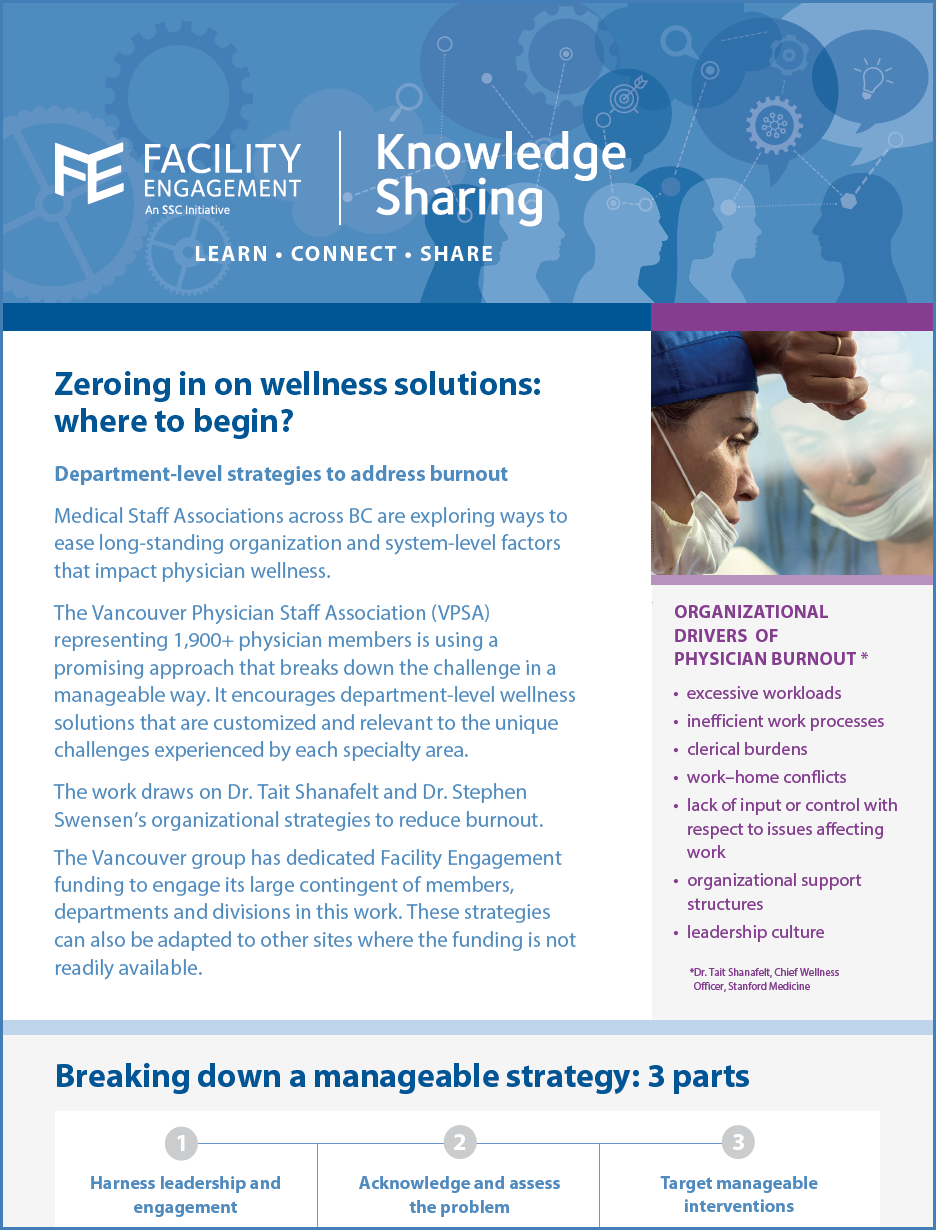
The Vancouver Physician Staff Association (VPSA) representing 1,900+ physician members is using a promising, evidence-based approach to break down the challenge.
It is encouraging department-level wellness solutions that are customized and relevant to the unique challenges experienced by each specialty area.
The work draws on Dr. Tait Shanafelt and Dr. Stephen Swensen’s drivers of burnout.
FEI funding has been dedicated to engage the large contingent of members, departments and divisions; however, strategies can be customized to smaller sites where the funding is not readily available.
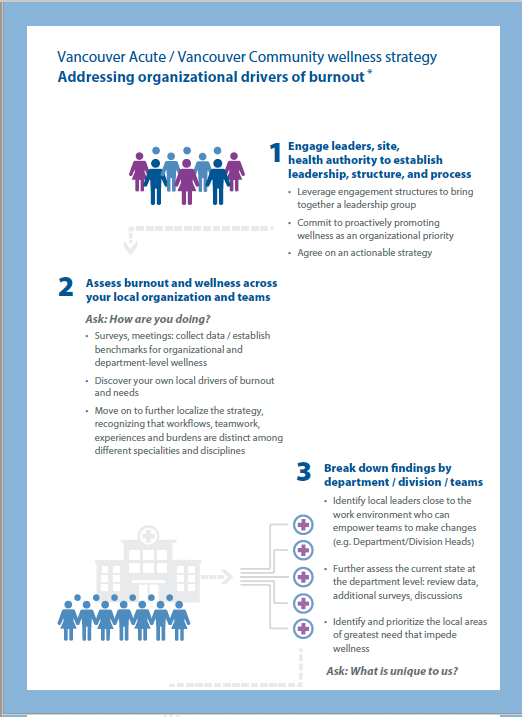
Vancouver Coastal Health (VCH) and the Vancouver Physician Staff Association (VPSA) joined forces in 2019 in the Vancouver Acute/ Vancouver Community (VA/VC) Physician Wellness Steering Committee to assess the level of burnout among physicians, find its causes, and develop collaborative solutions.
Physician leads were identified to champion the work.
- ED physician and steering committee co-chairs: Dr Zafrina Poonja and Dr Ka Wai Cheung
- Department heads: Dr Heather Lindsay and Dr Chris Lee
VA/VC surveyed their 1,900-plus physician members to understand what drives physician burnout and how that is different in every department. They analyzed the results, and started arranging further meetings with department and division heads to determine next steps.
Department and division heads can review their survey results and access engagement funding to further discover what specific burdens/barriers are impeding physician wellness and contributing to burnout in their specialty area. From there, they can develop data-driven interventions specific to their needs.
Applying the strategy in the Emergency Department
Four physicians volunteered as wellness champions: ED physician and steering committee co-chairs Dr. Zafrina Poonja and Dr. Ka Wai Cheung; and department heads Dr. Heather Lindsay and Dr. Chris Lee.
An interdisciplinary wellness team that includes physicians and nursing leadership meets once a month.
An ED-level departmental survey assessing physician wellness was conducted with the nursing team planning its own departmental survey.
Dr. Zafrina Poonja: Shifting mindsets
“Our group had the highest response rate to the survey. We knew burnout was prevalent before the pandemic and that it was only going to get worse with COVID-19. Our burnout rate has skyrocketed over the past 18 months. The department realizes it needs to recover from its baseline rate plus the added stresses of the pandemic. We need to act now to ensure recovery.”
“Our role is to try to understand the best way to advocate for our own physicians in a challenging environment. We need to shift the mindset to realize that when we look after ourselves better, we can better look after our patients. This needs to be done in a holistic way: as individuals; as a department; and advocating for the rest of the system. We need to identify and voice our concerns.”
Dr. Ka Wai Cheung: Identifying issues
“Every physician is in some way a wellness champion. Every shift, my colleagues and I are identifying issues to look into and finding appropriate ways to address these. We’ve all experienced burnout and know there are things that can be done. Some are easier than others; we’ve also identified systemic areas that will require more work.”
The group identified and started work on
multiple improvement initiatives in the
workplace to support ED physician
wellness. Examples include:
• improving the relationship between ED physicians
and consultants
• arranging more streamlined outpatient clinics
• changing how shifts are scheduled
The group identified multiple quality improvement initiatives that are underway to improve ED physician wellness.
Examples include:
- improving the relationship between ED physicians and consultants
- arranging more streamlined outpatient clinics
- changing how shifts are scheduled
Further plans to explore include:
- optimizing space within the department that the group feels it can address
- applying for funding to address some of the deeper systemic issues that are drivers of burnout (e.g., workload) and identifying champions to lead these
Dr. Poonja:
“Some radiology processes were not efficient from our perspective. We organized a meeting with the department and now things are running more smoothly.”
The work is still in early stages. While the micro interventions are helpful, major stresses remain overwhelming.
Some interventions may be within the control of the department, while others require change at organizational and system levels.
Dr. Poonja:
“We use Dr. Tait Shanafelt and Dr. Stephen Swensen’s list of drivers of burnout to assess how we’re doing. We’re doing well in terms of a sense of community within our group; we have a number of interventions in place for this. Patient load and administrative work are higher burnout drivers for us. Our survey has provided us with specific examples of this and we’re looking to categorize these results to see what we can take on.”
“I tell myself how much worse things would be if we hadn’t taken these steps.”
Dr. Cheung:
“Burnout has been a systemic problem for healthcare providers for a long time, but the stresses of COVID have been an extra burden. As frontline workers, we’re often the first to feel the burden but we don’t need to stay silent. There is a lot that can done. We can tackle this head on to the benefit of our colleagues and our patients.”