How are we engaging for physician wellness?
Explore and adopt engagement strategies from across BC
- Examples of Facility Engagement funded activities implemented through Medical Staff Associations (MSAs), Divisions of Family Practice, and with health authority partners to support well being and reduce burnout among physicians (2017-2024). Source: Site Engagement Activity Tracker, SRRP Submissions)
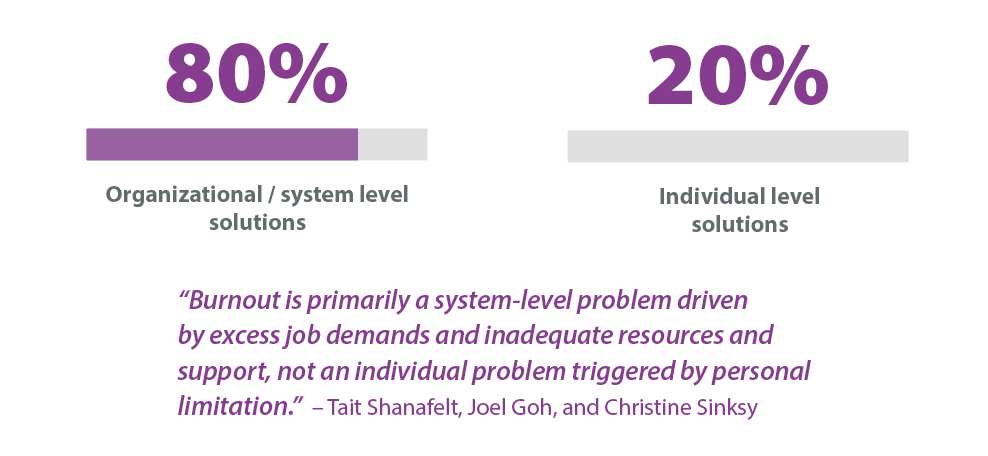
Physician wellness advocates suggest that about 20% of burnout is impacted by individuals, while as much as 80% is impacted by organizational/system factors that also affect the practice environment.
To maximize physician well-being, both individual and organizational/system level strategies are needed (West, Dyrbye, Erwin, & Shanafelt, 2016).
Facility Engagement recommends that MSAs focus physician wellness activities primarily in areas of the local work group-level and organizational-level improvements or in combination with individual level strategies.
MSA ACTIVITIES TO SUPPORT WELLNESS
APPRECIATION AND CONNECTION
Cranbrook: The Kudos Project at East Kootenay Regional Hospital is boosting physician well-being and strengthening workplace bonds through peer appreciation. The project has been adopted by other MSAs across BC. Learn more>
Campbell River: The Spirit Awards collaboration between the Campbell River MSA and Division of Family Practice celebrate local health care staff to reduce burnout and empower team members. Learn more>
Abbotsford: “Story Rounds” at the Abbotsford Regional Hospital and Cancer Centre give physicians from multiple departments an opportunity to share experiences about their work as a physician. Participants share stories of kindness, hope, challenge, compassion, humour, vulnerability, grief, and growth to help create a safe environment for physicians to discuss well-being and learn strategies to address burnout.
Vanderhoof: The physician lounge project at St. John Hospital has invigorated a space for physicians to work privately and connect with colleagues, through a partnership between the MSA, hospital staff, and health authority operational leaders.
Sechelt: Docs for Docs Workshop. A dialogue on physician mental health and their work environment aimed to create a supportive workplace where physicians can receive and provide the care for each other that they give so diligently to their patients.
Vancouver: Facilitated Dinner Groups organized by the Vancouver Physician Staff Association bring together physicians from across specialties to discuss common issues such as work-life integration, and to build peer-to-peer support in a facilitated environment.
Vancouver: Empowering Physician Self-Efficacy. A Balint Group at BC Children’s Hospital aims to improve physician psychological self-efficacy and physician wellness, and physician relational skills – including awareness of transference – to improve patient care.
PEER SUPPORT
Thinking about developing a peer support program? Reach out to the Physician Health Program at www.physicianhealth.com for training and knowledge sharing opportunities and to enable coordination of peer support initiatives provincially.
Prince George: The Doctors of BC Physician Health Program (PHP) Peer Support Program has supported the medical community to identify eight physician peer supporters who are helping other physicians experiencing work or life-related stressors that impact their well-being. Learn more>
White Rock: Peer support training at Peace Arch Hospital is provided by a psychologist specializing in physician peer support. It is available to any physician to any physician wanting to learn skills in effective communication, coaching, and support colleagues who are experiencing challenges in the profession.
Burnaby Hospital: Peer Support and Personal Resiliency Workshops organized by the Burnaby Hospital Medical Staff Physician Society Wellness Committee provide education sessions on peer support, communication skills, and managing personal energy, in order to promote collegiality, peer support, and personal self-care.
New Westminster: Confidential peer support at Royal Columbian Hospital provides a confidential conduit for individual physicians to contact an emotional first aid counsellor at Fraser Health. Each department identifies a trusted physician liaison who can be contacted in confidence to discuss acute emotional stress, and to be connected further with a counsellor.
Vancouver: The Medical Staff Peer-to-Peer Support Program at BC Children's Hospital and Women's Hospital provides accessible, in-house peer support to promote a psychologically healthy workplace, and training and opportunities for medical staff to engage with peers to provide support.
Vancouver: The Young Faculty Initiative at BC Children's Hospital and Women's Hospital provides group mentorship support for newer faculty members through regular structured meetings. Members discuss a variety of topics relevant to professional, academic and personal endeavors. Each session is moderated by a senior physician with experience in the area, or by an external speaker.
COURSES AND SEMINARS
South Island: A Narrative Medicine Workshop and Writing Group, supported by the South Island MSA and South Island/ Victoria Divisions of Family Practice, is a group of physicians who share the desire to practice narrative medicine writing skills with a group of like-minded peers, in a supportive and facilitated way.
Vernon: “Us Care” – Civility Matters Project at Vernon Jubilee Hospital has provided education and tools for physicians and hospital staff to overcome the profound downstream impact that rudeness in the workplace can have on recipients of uncivil behaviour on witnesses to the event, and on patient care. Learn more>
Nelson: Mental Health and Resiliency Workshops at Kootenay Lake Hospital include a series of mental health/resiliency-focused and facilitated virtual workshop sessions to equip physicians with insights and tools to support resiliency in the workplace.
Vancouver: Physicians Staying Humane in the ER explores the causes of stress and burnout, with an aim to create civility, collegiality, humanity in the workplace, and restore joy and compassion in the emergency room.
Kootenay Boundary / Cowichan: Compassion Training (CCT) organized by the Division of Family Practice included two series of Stanford University-developed training for physicians and other care providers (including midwifes and nurse practitioners). Participants rated the training as outstanding.
Kootenay Boundary: Resiliency Rx Sessions - The Division of Family Practice partnered with the Kootenay Boundary Family Residency Program to invite residents and staff to participate in short sessions about resiliency, facilitated by a local psychologist. It included a series of text-based check-ins to loop back on key learnings.
ADDITIONAL SEMINAR OPTIONS
Thrive Resilience and Well Being Coaching Program for Docs: Tools and strategies to manage both the everyday hassles and big challenges. Learn more>
Burnout Proof Life Workshop for Physicians: Training to recognize and deal with burnout on a personal and organizational level. Learn more>
Linda Edgecombe: Kindness and Humility in Crazy Times: A humorous, motivational speaker with an expertise in resiliency training reminds people to tap into their sense of humour to find ways to recover their sense of balance. Learn more>
BC Cancer Agency: Human resource planning, capital planning, equipment and operational capacity planning among radiation oncologists aims to address anxiety-causing issues.
Vancouver: An assessment of current obstetric internal medicine service demands at BC Children's and Women's Hospital includes future planning to avoid burnout from escalating referral volumes.
Kelowna: Accreditation for an Associate Physician (AP) Program for the BC Associate Physician (AP) Program has led to the hiring of four new AP physicians who have joined the Kelowna General Hospital Hospitalist Service, with other services to follow. More information>
Across BC: Reducing issues around electronic health record (EHR) Implementation: Physicians and health authority leaders are collaborating to overcome issues and develop solutions to reduce stress experienced during technology adoption. Supportive MSA / health authority partnerships have been created across the province, such as the BC Cancer Agency/VCH CST, Cowichan District Hospital/IHealth, and Interior Regional EHR table. More information>
Hazelton: Operating Room (OR) enhancements at Wrinch Memorial Hospital aim to improve the surgical services program by enabling family physicians to utilize the OR space to perform procedures with the help of OR staff. Monthly working group meetings held jointly with Emergency Room (ER) and OR participants focus on ER-OR alignment, organizing simulations, and training.
Cranbrook: Inpatient Congestion and Flow project at East Kootenay Regional Hospital (EKRH): aims to create realistic recommendations to reduce inpatient congestion (over capacity).
Prince George: An internal medicine specialist and family doctor collaboration at the University Hospital of Northern BC supported better communication, and set expectations between family physicians and internists while increasing inpatient coverage.
Creston: A shared Maternity Clinic at Creston Valley Hospital is more coordinated, integrated with Public Health, consistent between providers, and includes a call group that allows for more flexibility. Implementation of weekend ward rounds in the emergency room with family physicians and nurses streamlines the chart review process and saves time. Learn more>
New Westminster: A Crucial Conversations course at Royal Columbian Hospital provided tools to build clear, consistent, and respectful communication between a wide variety of providers, to help identify opportunities for improved quality of care and the workplace environment. Learn more>
Fraser Health: Coordinated cross-region wellness strategies across 12 MSAs and ten divisions of family practice are engaging peers, partners, and Fraser Health to build a culture of wellness starting at the grassroots level, and influence organizational /system-level change to support wellness. Activities include events, workshops, community wellness teams, safe spaces, peer mentoring, compassionate leadership training, and funding support from Fraser Health.
Vancouver: The Medical Staff “People” Pillar at Providence Health Care includes medical staff leaders and representatives paired with senior health authority partners. Together, they support and promote medical staff wellness as a strategic organizational priority, through increased health authority wellness and safety strategies, and medical staff connection opportunities focusing on building relationships and community, and supporting well-being.
Burnaby: A formalized engagement process for health care operations challenges at Burnaby Hospital enables medical staff to engage and align with local and regional administration leads to address health care operational challenges that affect providers and patient care.
Vancouver: MSA-HA Wellness Committee activities organized by the Vancouver Physician Staff Association support wellness among medical staff with guest speaker events, a new Regional Medical Director position to operationalize physician wellness in partnership with Vancouver Coastal Health, targeted clinical department wellness funding, Commensality Groups, and adoption of the Kudos Project to recognize medical staff. Learn more>