Photo left: Elder Helen Buzas of Lhedli T’enneh, Indigenous Health Service Assistant, UHNBC – a new role resulting from the Prince George Medical Staff Physician Association Emergency Department engagement project.
How are we engaging on this project?
UHNBC is uniquely positioned to address health inequities affecting Indigenous Peoples. The region has the highest Indigenous population in the province. It is also the largest teaching hospital in the north for health care providers of the future.
Building towards more equitable and culturally safe care is a key priority Prince George Medical Staff Physician Association (PGMSPA) and Northern Health, who have supported an Emergency Department (ED) project to create more culturally safe care in the ED – often the first point of entry for individuals accessing medical care and when they are most vulnerable.

To lead the project, Dr. Christina Boucher, a non-Indigenous ED physician, partnered with Elder Lucy Duncan and UHNBC leadership including Courtenay Kelliher, Manager of Clinical Operations.
The project was supported by Northern Health and the Prince George Medical Staff Physician Association through Facility Engagement.
They invited Elders and Indigenous community members with lived emergency care experiences to join interdisciplinary health care providers in monthly meetings.
Before jumping to solutions, they prioritized building understanding and uncovering a common purpose through truth-telling and the sharing of personal stories.
Building on a foundation of relationships and community connections, the advisory group advanced practical recommendations for improving cultural safety in the ED as well as other areas of the hospital.
Northern Health took concrete action to implement changes, ranging from hiring new Indigenous Patient Navigators, to making the hospital space more culturally welcoming.
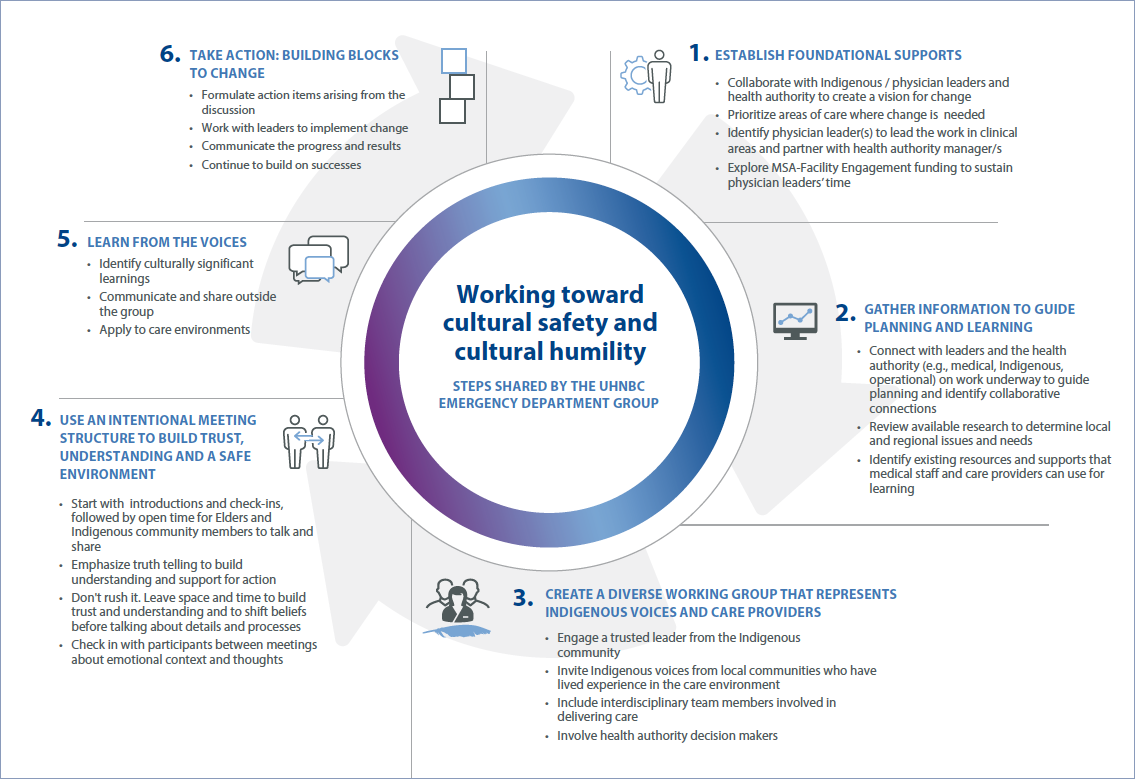
Dr. Boucher, Elder Lucy Duncan, and Courtenay Kelliher share their steps to building positive change, below.
Knowledge Sharing: Steps to Action
In 2018 when Dr Terri Aldred pioneered the PGMSPA’s Cultural Safety and Humility work (subsequently led by Dr Todd Alec).
In 2019, emergency department physician Dr Christina Boucher connected with Dr. Aldred to help guide a new cultural safety and humility project in the UHNBC Emergency Department (ED).
She sought funding for engagement from the Prince George Medical Staff Physician Association through Facility Engagement.
Dr Boucher is an ER physician at UHNBC and a non-Indigenous person who seeks to be an ally and advocate for issues of inequity in health care delivery concerning Indigenous people.
To gain context about cultural safety issues in the health care system, Dr Boucher referenced two key resources:
• A review of the EQUIP research to better understand specific health equity issues in the ED. (The EQUIP research provides insights for EDs across BC.)
• Insights from In Plain Sight “Addressing Indigenous-specific Racism and Discrimination in B.C. Health Care” that reports on issues of inequitable health care access and outcomes endured by Indigenous peoples in BC health care settings.
She also connected with work underway, and initiatives and resources offered by Northern Health’s Indigenous Health team to support learning and self-reflective practice among all physicians and employees.
Elder Lucy Duncan
A key support create a foundation for relationship-building has been the engagement of Lucy Duncan, an Elder working at the Central Interior Native Health Society, and contributor to the EQUIP Health Care work which seeks to ensure health equity within BC’s health care system, and who further spread the word to Indigenous community members to add their voices.
Elder Lucy Duncan is a member of the Binche Whu'ten Nation belonging to the Lhojuboo (Bear) Clan. She works with Central Interior Native Health as an Elder and provides cultural education to health providers and medical students. She initiates a safe space for clients such as cultural practices, spiritual guidance, family support, and connects people with other health or community resources.
She also contributes to EQUIP Health Care work to foster health equity within BC’s health care system.
Elder Lucy has been an enthusiastic and key partner on the ED project to bring Indigenous community members' perspective to planning for more culturally safe care.
Creating a collaborative, diverse advisory/working group with Indigenous voices and interdisciplinary providers
• With Elder Lucy, the partners identified all vested voices needed to come together, source and articulate issues, work together on solutions, and foster and sustain change.
• They included and invited trusted voices from the Indigenous community and members who rely on the ED and who have lived experiences with care in the ED.
• In the hospital, they engaged of all interdisciplinary positions working in the ED, and health authority managers.
Advisory Group members
• Elder, Central Interior Native Health Society
• 2 MSA physicians
• Northern Health staff: ED Program Leads (x2), Social Worker, ED Nurse, Acting ED Manager
• Indigenous Psychiatry Resident
• Indigenous patient
• Indigenous artist
• College of New Caledonia Aboriginal Resource Centre representative
• Former Chief, Stellat’en
• Elder Teacher, Lheidli T’enneh
• Aboriginal Patient Liaison
• Central Interior Native Health Services, Nurse Health Care Coordinator
• University of Northern BC / EQUIP researcher / Nurse Practitioner
Feeling and finding purpose through truth telling
At monthly meetings, group members focused on creating an authentic foundation for change, through:
Using an intentional meeting structure that emphasizes connection before content. Meetings start with introductions and check-ins, followed by open space and time for Elders and Indigenous community members to talk and share.
Emphasizing the importance of truth-telling to build understanding and support for action to address Indigenous-specific inequities in care.
Creating space and time to build trust, create understanding, and shift beliefs before talking about details and processes. Talking about cultural safety and cultural humility can be challenging on a social and emotional level, and cannot be rushed.
Checking in between meetings with working group members about their thoughts and feelings, as each will react differently as personal and emotional stories are shared.
Forming action items arising from the discussion.
How did Northern Health take action? What changes were made in the ED and hospital?
Courtenay Kelliher, Manager of Clinical Operations at UHNBC, stepped in to oversee implementation of changes.
New Indigenous support roles
• Northern Health hired three full-time Indigenous Health Service Assistants to support patients arriving at ED. As part of the interdisciplinary team, the assistants help patients with their comfort needs, navigating the ED, and making connections to their communities, while serving as a learning resource for physicians and frontline care staff.
• An additional Indigenous Patient Liaison was contracted through Carrier Sekani Family Services to assist patients in navigating their medical care and related needs if they are admitted to the hospital from the ED.
• New roles were also extended to inpatient settings, including two additional Indigenous Health Service Assistants, and an Indigenous Care Coordinator with a social work background to support family meetings, discharge planning, and connections to Indigenous Health resources.
• Notably, the hiring process for these positions involved Elder community members, who helped develop interview questions, assess candidates, and make the final hiring decisions.
Improving the hospital environment
• The ED environment was made more welcoming to the Indigenous community with Indigenous artwork and a display drum which can be used for in-hospital drumming ceremonies – both completed by local Indigenous artists.
• There is also work underway to add bilingual signage, translated by Elders from English to Dakelh, to the ED.
• Northern Health relational security officers underwent extended cultural safety training and consulted on plans to make their uniforms more culturally appropriate and welcoming for patients, families, and visitors arriving at the hospital.
• UHNBC amended its scent-free policy to allow for essential-oil liquid smudging in higher-acuity areas like the ED, and established a comforting viewing space for Indigenous families whose loved ones have passed, and where full smudging ceremonies can be performed.
With many recommendations implemented, the ED advisory group meets less frequently, while maintaining virtual connections. Members are ready to be involved in new projects, such as upcoming plans to make the chapel space more culturally accommodating.
Northern Health Cultural Safety and Humility offerings (a snapshot): www.indigenoushealthnh.ca
• Cultural Safety Implementation Framework and System Change Assessment Tool for the organization to embed cultural safety and humility across the organization.
• Ongoing partner work with the Northern First Nations Partnership Committee and opportunities for communities to submit funding proposals related to community-based health, holistic health and bringing Indigenous knowledge into these opportunities.
• Videos narrated by Dr Evan Adams: ‘Compassion Informed Care.’
Check out the Doctors of BC Guide for Respectful Indigenous Engagement to support divisions, MSAs, and physician members in their work with First Nations, Métis, and Inuit.
“This process has been very important from a systems perspective. We've always tried to make changes that never worked. We have never been heard before or listened to. The meetings with providers listening to us made a big difference.” – Elder Lucy Duncan
“The challenge is to be sure you are working on the real issues that will make culturally significant change – so it’s important to verify with the community.” – Dr Christina Boucher
“We’ve come so far. There’s more and more support. Indigenous patients are saying they feel a lot more supported, and safe, in the care that they're receiving. They know who they can go to.” – Courtenay Kelliher