"Change is more effective when you've got united voices, and when we have the issues clearly identified so that we can figure out how to fix them.” - Dr Trina Larsen Soles
(Photo: L to R: Committee members Katherine Cowan, Dr. Todd Loewen, Dr. James Heilman)
Patient transportation in the East Kootenay (EK) faces challenges due to geography, highways, weather, resource constraints, and jurisdictional boundaries.
A regional Facility Engagement committee spanning five hospitals - Fernie, Creston, Invermere, Golden, and Cranbrook - has brought together MSAs, Interior Health, and partner organizations to better understand and address issues – and ultimately improve patient care and experiences, and provider experiences.
One primary focus is to enhance the capacity of rural East Kootenay sites that refer patients to East Kootenay Regional Hospital, including to provide care for complex patients and reduce the need for transfers, through changes such as managing agitation in the ER.
Our story: taking regional action
The East Kootenay Patient Transportation Committee has brought together local, regional and provincial stakeholders for change. Since starting, it has has evolved from a sounding board into a collective, united voice, with:
- relationships and communications channels among stakeholders;
- a better understanding of the pressures, the health care system and how to navigate it; and
- a regional approach to address common barriers and challenges to improve both patient care and provider experiences.
Uniting voices for action
A regional committee was formed with eventual representation from:
- The five hospital’s Medical Staff Associations (MSAs) - Fernie, Creston, Invermere, Golden, Cranbrook
- Physician clinical leaders
- Interior Health clinical and administrative leads, including the regional High Acuity Response Team (HART)
- BC Emergency Health Services (BCEHS)
- Other stakeholders.
The group took steps to define their scope and ensure a manageable approach to the work.
1. The first, foundational work was to conduct a scan of the current work happening in patient transportation locally, regionally, and provincially.
That included a review and analysis of the 2016 Rural Patient Transport and Transfer Research Report. The committee looked at the report’s 18 recommendations to determine where they could influence and make changes.
2. This was followed with an East Kootenay Roadshow called Patient Transportation 101 – where input was sought from MSAs and local hospital administrators to learn about their pain points, opportunities, and challenges. In addition, regional meetings were held with BC Emergency Health Services.
The Committee built out their strategic priorities based on this upfront collaborative work.
- To build the Committee’s knowledge and understanding of the issues impacting patient transportation in the East Kootenay (EK) region and disseminate this information across EK facilities to build knowledge and capacity.
- To effectively measure the current state of patient transportation in East Kootenay and identify the key factors of what is working and what is not.
- To build and support the capacity of interdisciplinary teams at the rural sites to maintain care of more complex patients in order to reduce transportation needs and overcapacity at the regional site.
- To cultivate a collective voice of East Kootenay medical staff and regional stakeholders to inform and influence policy makers.
In 2019, plans were being developed to identify trends and problems areas at all EK rural sites, begin collecting data on patient transfers and identify available educational opportunities and spread to other sites.
While this work was getting underway – COVID arrived causing a pause until 2021. In spring 2021, the committee regrouped and reassessed priorities and emerging issues.
Following the COVID-19 pause, rural sites in particular were noting an increase in acute mental health and substance use cases, combined with a shortage of psychiatrists in the East Kootenay region.
The issue was brought back to the regional committee.
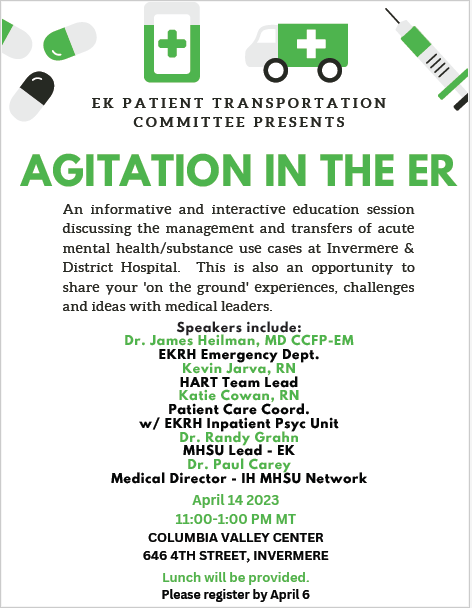
In 2022, with additional funding support from regional Facility Engagement, the committee started working to build capacity to support the rural sites and build relationships with the regional hospital by holding Agitation in the Emergency Department sessions for rural site physicians, allied health, and administrators.
The sessions, organized in collaboration with mental health/substance use leaders at Interior Health also provided an opportunity to:
- increase rural provider knowledge about the mental health act, procedures, forms and best practices when managing highly agitated patients and
- to allow health authority leaders to hear first-hand about current issues facing the rural sites, to escalate for regional solutions.
The path forward, together
Dr Trina Larsen Soles, Committee Member
"Issues still exist, but the difference is we now have a path to continue to make things better. These solutions happen because we are working together.
It boils down to three things. It’s about communication. It’s about relationships, and it's about trust. The more that we work together to communicate around these issues – and the better the relationships get, and the more we can trust each other that we're all focused on doing the right thing for our patients.
We need to change the infrastructure, obviously. But change is more effective when you've got united voices, and when we have the issues clearly identified so that we can figure out how to fix them.”
Kevin Jarva, Committee Co-Chair and High Acuity Response Team Lead for East Kootenay
“Facility Engagement has allowed for a collaborative multi-disciplinary forward-thinking approach to creating change in the way we deliver healthcare in the constraints of a challenging rural environment.
This committee has made improvements that are leading to better patient outcomes and better health for all.”
Dr Todd Loewen, East Kootenay Senior Medical Director
"This regional approach to patient transport challenges facilitated through Facility Engagement has brought all corners of the EK together in a manner not previously possible.
This has created a “collective voice” around transportation concerns that is not only the physician perspective but also that of local IH and EHS leadership.
We are reassured the message is getting through and that efforts toward positive change are ongoing."

L to R: Patti King, Engagement Partner DoBC, Dr. James Heilman, Dr. Randy Grahn (IH MHSU Lead for EK), Gail Gross (Project Manager Invermere), and Katherine Cowan. (Invermere education session)