How are MSAs, physicians and the health authority engaging in Northern Health?
Physicians and health authority representatives from 11+ Northern Health hospitals share engagement successes, priorities, and an ideal future state.
Learn and adapt ideas from the Northern Region Facility Engagement Conference.
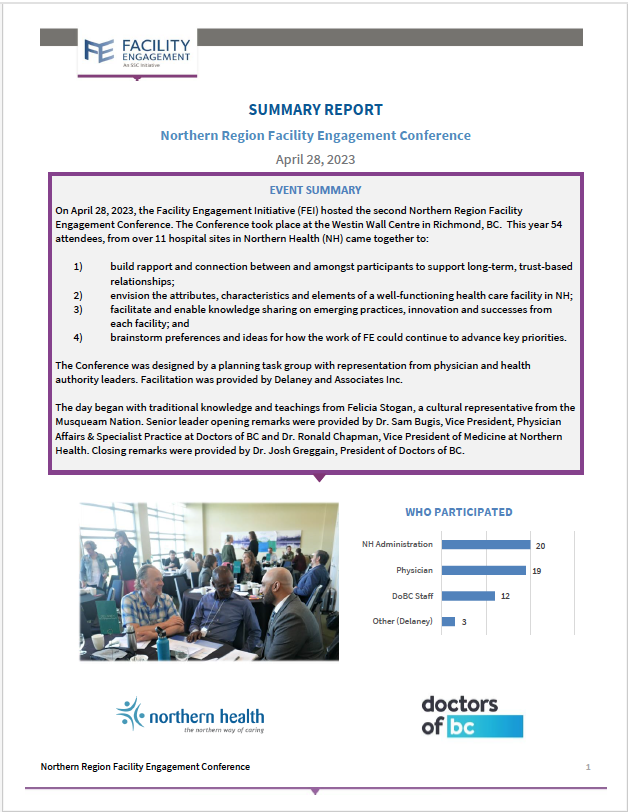
In the spring of 2023, 19 physicians and 20 health authority representatives from more than 11 hospital sites joined together for the Northern Health (NH) Facility Engagement Conference to share, celebrate and look to the future of engagement. Discussions included:
- how to build rapport and connection between and amongst participants to support long-term, trust-based relationships
- discussion of the attributes, characteristics and elements of a well-functioning health care facility in NH
- knowledge sharing on emerging practices, innovation and successes from each facility
- brainstorm preferences and ideas for how the work of FE could continue to advance key priorities
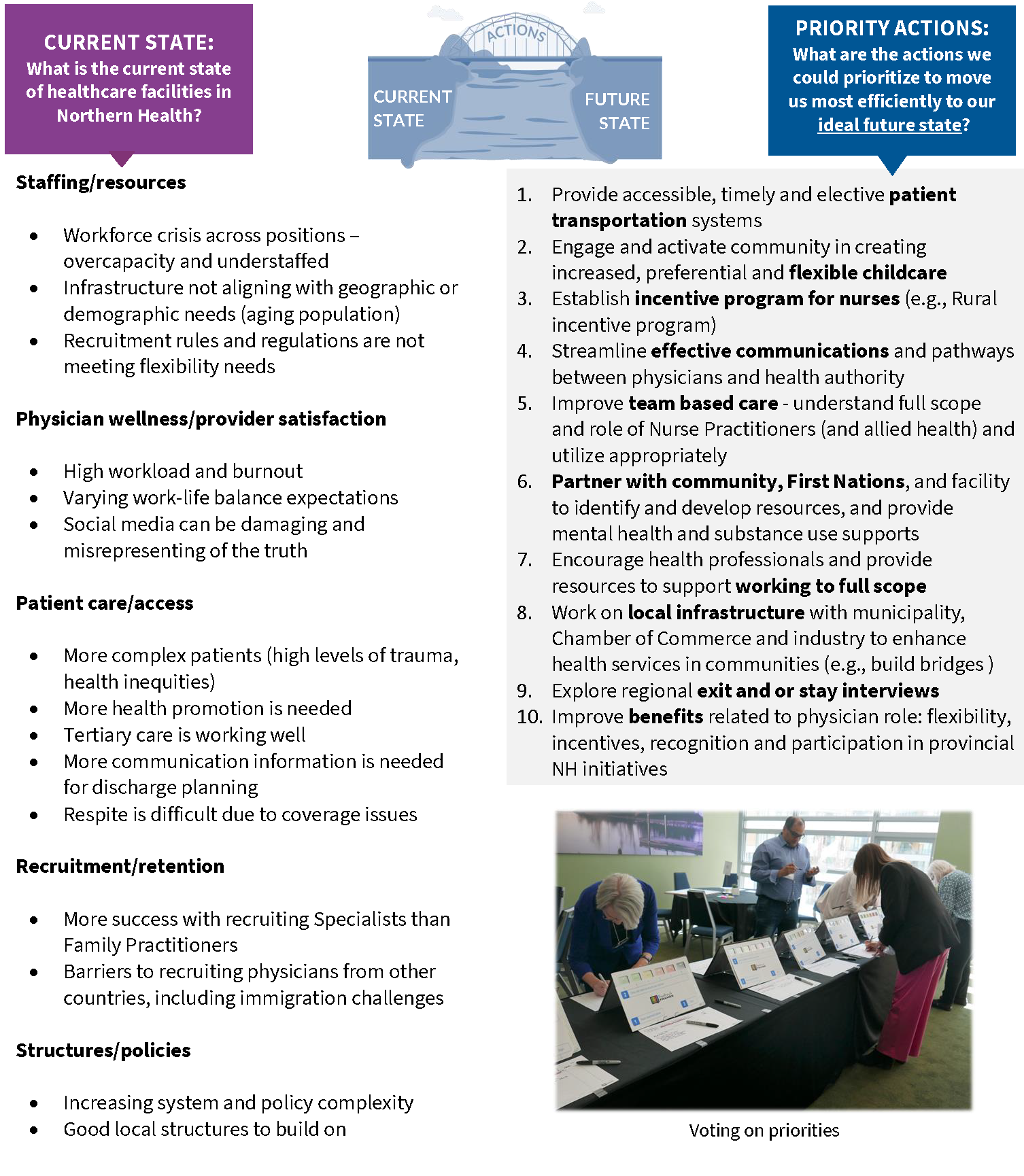
Creating an ideal future state
Key Takeaways
Takeaways: what is most important?
- Recognition of ability to influence and create change
- The power of coming together in-person to problem solve
- Learning from our peer communities and sharing successes
- Identifying shared priorities across the region
Actions: how do we get there?
- Community-based problem solving
- Collaborating
- Changing culture: shared vision
- Building trust
- Connecting & building relationships
- Communicating
Insights, ideas & opportunities
- Developed an onboarding program that helped new physicians know how to reach out, complete IT tasks & learn about what the community has to offer.
- Practice Ready Assessment (PRA) program introduced to help with physician shortages.
- Expansion of residency program planned for the near future.
- Completed many exit interviews and found that factors outside of Northern Health control were most common for departure.
- Learned a lot through COVID on patient transport – business model is being proposed for services and supplies.
- Supported a number of activities to help move the needle on cultural safety and humility, such as carving of a totem pole, monthly Elder teachings, master glossary creation and more.
- New Communications Lead in Medical Affairs hired by Northern Health.
- Terrace specialist model with specialists in rotations
- Intentional fast response to Health Match BC
- Having a compelling vision, which is communicated well with stakeholders
- Network of services – coordination of Health Service Delivery Areas (e.g., surgical days)
- Interdisciplinary bundled care for patients (e.g., breast cancer) and at same cost
- Encouraging autonomy, purpose and passion leading from learning and innovation
- Creating a medical ecosystem
- Helping new medical staff to connect with the community
- Informal mentorships on site
- Weekly formal team building activities
- Listening and dialogue – allowing innovation and space to learn
- Team-based care (e.g., Registered Nurse integration increases quality of care efficiency)
- Training Nurse Practitioners as surgical assistants and pre-post operative care, to reduce surgical cancellations
- Having strong local level leadership
- Increasing leadership training opportunities for physicians
- Increasing awareness and opportunities for cultural safety and humility training
- Recruitment and retention strategies
- Expansion for support of allied health participation in FE funding guidelines
- Physician wellness and team building
- Communicating outcomes and learnings with broader MSA physicians and partners
- Onboarding new physicians to Facility Engagement
- Patient transportation
- Information Management
- Building partnerships outside of Northern Health
- Supporting 2-way dialogue and a common vision between medical, operational leadership and the MSA
- Providing a pathway to influence where items are not in direct control
- Continuing to support relationship-building
- Increasing awareness of MSA and FE function and how they can support physicians
- Gathering information and best practices on overcapacity issues related to lack of transport. Aim to translate findings into action for: advocacy, knowledge sharing and building relationships with the Northern community
- Partnering with Ministry of Health, HA and MSA to have a provincial voice and address collective issues
- Partnering in community
- Continuing communication and transparency
- Collaborating across the region and building strength in numbers