"We can't fix overcapacity in a meaningful way without getting more long term care. – Dr Barb Kane, Psychiatrist and Northern Health’s Medical Lead for Mental Health
"We can't fix overcapacity in a meaningful way without getting more long term care. – Dr Barb Kane, Psychiatrist and Northern Health’s Medical Lead for Mental Health
A regional Facility Engagement project that engaged health authority leaders, administrators, data analysts, and physicians from MSAs in 11 Northern Health hospitals has validated a common issue.
Long-stay patients waiting for community services or beds significantly contribute to overcapacity in their hospitals, a daily challenge that impacts patient access to emergency, surgical, and other services. Dr Barb Kane shares data-driven recommendations, actions, and a data tool for other sites and health authorities to use.
Our story
Watch: Dr. Kane's presentation - Sept 2023 Peer-to-Peer Round Table
PRESENTATION TAKEAWAYS
Impacts of Long Stay Patients on Hospital Overcapacity
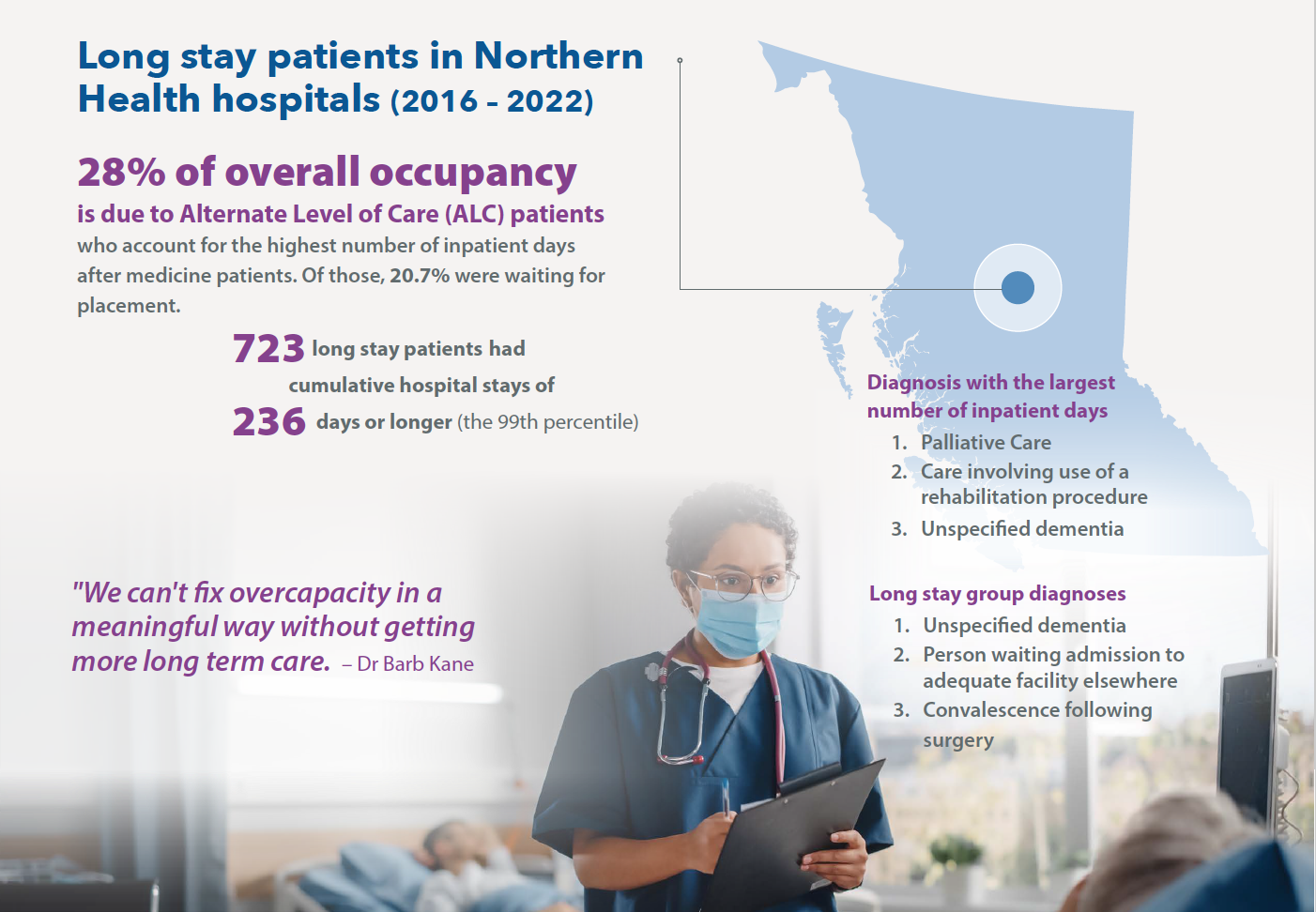
The Northern Health Hospital Overcapacity Analysis regional engagement project has validated the impacts of long stay patients on hospital overcapacity.
- As the Medical Lead for Mental Health in the University Hospital of Northern BC, Dr Barb Kane was aware that daily overcapacity in the hospital was a significant concern; sometimes as much at 25%.
- Data analysis from 2016-22 revealed that 11% of patients had a length of stay over 30 days, contributing to 55,000 excess bed days.
- This insight inspired Dr Kane to lead Facility Engagement's first regional project to determine the impact of long-stay patients across Northern Health.
- It involved a cross-disciplinary working group with a wide range of perspectives, and engagement of many of the smaller hospitals and medical staff associations across the region to capture feedback from physicians around their experiences.
- The health authority provided in-kind support including data analysis experts, who identified that palliative care was one of the leading diagnoses for long stays. Notably, ALC (Alternative Level of Care) placements were a significant factor in overcapacity, accounting for 28% of bed days.
- The insights led to implications for resource allocation, highlighting the impact of long stays on elective surgeries and emergency services, and delays and access issues.
- More long-term care beds were identified as one critical solution to address overcapacity effectively.
- Northern Health is using the findings to enhance a number of current actions in the community, and to inform future plans.
- The project's supports for success included the Facility Engagement opportunity and funding for a regional project, routine stakeholder engagement, site-specific data, feedback from medical staff providing the care, and in-kind support from Northern Health.
PROJECT STEPS
- Dr Barb Kane, Medical Lead for Northern Health's Mental Health program, wanted to see what community resources were needed for patients with long stays on psychiatric wards.
- She soon discovered that long-stay patients overall make up a significant part of hospital overcapacity.
- Hospital overcapacity is a critical and daily problem for patients waiting to access care across BC, who experience emergency room overcrowding, hallway care, long waits for surgery, and canceled surgeries. It is also a cause of burnout among care providers.
- Observations in Northern Health have indicated that long-stay psychiatric, medical, and dementia patients contribute significantly to hospital overcapacity. Physicians confirm that alternative level of care (ALC) patients and those with a final diagnosis of palliative care make up a significant part of their work.
- To validate and better understand which diagnoses contribute most significantly to this issue, Dr Kane and physician and health authority collaborators joined together in a Facility Engagement regional project to investigate overcapacity in all departments and facilities across the region.
A Working Group with broad representation organizationally and geographically:
• Dr Barb Kane – Medical Lead, Mental Health Program, Northern Health (NH)
• Jess Place – FE Sponsor, Executive Lead, Regional Chronic Diseases Program, Northern Health
• Sherri Tillotson – Senior Operations Officer, UHNBC
• Kendra Kiss – South Peace Health Services Administrator (Dawson Creek), Northern Health
• Dr Ian Schokking – Family Physician, UHNBC
• Dr Andrew Deonarine – Medical Lead, Informatics, Northern Health
• Jordana Archer – Clinical Outcomes Analyst, Northern Health
• Jim Campbell – First Nations Health Authority
• Holly Hovland – Engagement Partner, Doctors of BC
Outreach to Northern Health sites and MSAs to seek local insight and represent physician voices.
Feedback from these sites and the Medical Advisory Committee, has been integral to the Working Group's analysis and recommendations.
• Bulkley Valley District Hospital – Smithers
• Chetwynd Hospital – Chetwynd
• Dawson Creek and District Hospital – Dawson Creek
• Fort Nelson General Hospital – Fort Nelson
• Fort St. John Hospital and Peace Villa – Fort St. John
• Lakes District Hospital and Health Centre – Burns Lake
• Mackenzie and District Hospital and Health Centre – Mackenzie
• Northern Haida Gwaii Hospital and Health Centre – Masset
• University Hospital of Northern British Columbia – Prince George
• Wrinch Memorial Hospital – Hazelton
- Facility Engagement (FE) Regional Funding
- Northern Health in-kind support from including: data analysis by an outcomes analyst assigned to serve on the project’s Working Group, and informatics expertise to co-develop the framework for data analysis, and create a program to segment data by health conditions.
- Project manager support via FE/Doctors of BC.
- Intentional, thoughtful, and routine engagement of stakeholders, representing different perspective and experiences.
- Getting on the existing agenda for MSA meetings, rather than creating a new meeting.
- Having site-specific data available for each of the hospital sites: including top 3 diagnoses, for a relevant discussion with meaningful feedback.
- Listening to perspectives on what physicians were dealing with on the ground - and impacts on their providers and patients - not just analysing data. This adds context and meaning to the data analysis.
- Using Zoom as a meeting tool to engage more people within their schedules: allowing for broad engagement across a significant geographic area.
Examples of physician feedback from 11 Northern Health sites
- "Out of 5 acute care beds, 3 to 4 were taken up by ALC patients" (small rural site in Dec 2022)
- "Having elderly patients in the hospital is far worse for the patient than in a LTC facility. There, they can give cognitive stimulation, family visits, and private space.”
- "There’s a six-month wait for a long-term care bed. Patients get ‘stuck’ - they can’t get into LTC, but they can’t go home, so they become palliative.”
- “When there is a patient backup, they have surgery waitlists – it’s a vicious cycle and everything is interconnected. You can’t look at this in silos.”
- "Discharge plans cannot be implemented because of the lack of community supports."
- "They can’t (discharge an unhoused psychosis patient) in -20° temperatures into the community, so they’re keeping him in hospital. There is no Social Worker, so I’m spending hours trying to find him a bed.”
- "Smaller sites face frustrations when there are no [mental health] beds in bigger centres to send their more critical patients or patients with psychosis that they don’t have the resources to deal with.”
- “Everybody is hoping that some other health authority will have a solution.”
- "If we could take long stay patients out, we wouldn’t need more acute care beds.”
Many long-stay patients are receiving care in hospitals because adequate long-term or specialized facilities are not available.
- The need for more long term care beds is at the heart of many long hospital stays. Patients wait in hospital until a suitable bed opens up.
- Rural and remote communities have massive challenges accessing services in the community.
- With limited nursing support, hospice services, or facilities in communities, patients at end of life can often only access palliative care services though their local hospital (even if they'd rather be at home), which costs the system more than palliating at home or in hospice, and is less desirable for many patients.
- The number of patients with a final medical service of palliative care and who died in a facility far exceeds the available dedicated palliative care beds.
- Being at the intersection of mental health, long-term care, and eventual palliative care, dementia’s impact on the overcapacity within Northern Health hospitals is significant.
- Convalescence following surgery: Without post-op recovery beds and local rehab services, the number of surgeries done per week must be reduced.
- Physicians at smaller sites particularly find themselves caring for patients who would ideally be cared for in a non-acute care setting, but whose medical condition combined with the lack of appropriate resources precludes them from being released.
Daily challenges of discharging ALC patients from local hospitalS
- Not enough available beds and other palliative care options
- Limited post-op rehabilitation resources
- A combined increase in mental health acuity and decrease in available services; compounded in rural communities
Services and facilities that provide optimum care for long-term patients needs to be a priority.
- Develop services for Palliative Care and Long-Term Care and Dementia Care for small, medium, and large communities, offering options that allow for local solutions (with funding to support implementation of locally-identified and developed solutions.)
- Identify ways in which the current home care structures, offerings, and staffing models can better support dementia patients and caregivers.
- Develop a new model of care for patients with Organic Mental Disorders, including consideration of community-based facilities designed and staffed to meet their specific care needs.|
- Develop new models of care for patients identified as Alternate Level of Care with resources to provide their care needs in a non-acute facility.
- Rethink models of care for the rehabilitation of post-surgical patients in smaller communities, considering scopes of practice of Allied Health providers, availability of Haealth Human Resources, and seasonal transportation challenges.
- Using local and provincial data, identify the business or service requirements needed to deliver safe, long-term care for patients with schizophrenia and other severe mental illnesses.
- Reconsider ways in which patients with Congestive Heart Failure can be better cared for in community, reducing the need for multiple re-admissions.
Northern Health is taking steps to address gaps in care, while the findings of the overcapacity project will continue to inform practical plans moving forward.
- Business planning is underway for a number of additional long-term care facilities across the North to increase capacity in the communities of Fort St. John, Prince George, Quesnel, Smithers, and Hazelton.
- Advancing rural alternatives in Dementia Care, such as Parkview Place and Aurora Home in Vanderhoof (https://connexus.ca/housing-services/). – A business plan is underway for a 12-room Alternative Dementia Housing project in Kitimat. Implementation is underway for a 10-bed dementia care home in Prince George.
- Broad implementation of DementiAbility and Gentle Persuasive Approaches (GPA) to manage responsive behaviors that often challenge staff. These two programs provide staff with tools and approaches that lead to improved dementia care.
- Improving the Home Support Program by increasing the availability and flexibility of home support, which will include expanding hours of service up to overnight, enabling people to avoid unnecessary hospitalization and facility-based care.
- Pursuing Transitional Care Options for short-term, transitional housing for those needing additional support after a hospital stay, prior to returning home. There are four units planned to open in Prince George in fall 2023.
- Implementing an Alternative Level of Care Designation policy that expects assessment for long term care to happen in the most familiar environment (home) whenever possible and all avenues to safely discharge from the acute care setting are explored using cross-functional teams from different parts of the health system (community, acute, physicians).
- Implementing a 12-bed Hospital@Home Program at UHNBC, in which eligible, stable patients receive hospital-level care in their home, rather than in an actual hospital facility. Care is provided 24 hours a day, 7 days a week, and 365 days a year and the patient may be pre or postoperative.
- Established a quick response team (QRT) in the UHNBC emergency department and on the inpatient units. This is an inter-professional team that provides an early coordinated response to support patients who have complexities but do not require an acute level of care to either avoid admission or ensure timely discharge.
- Expanding Adult Day Care Service in Prince George. Increased adult care service spaces by 25, added a community bathing program.
- Implemented 7/7 extended hour community care integration coordinator working alongside the patient care coordinator at UHNBC for 7 day a week flow.
- Implementing a Ketamine Clinic and an rTMS clinic in Prince George for the treatment of depression.
- Planning services that help reduce overcapacity: Mental Health Day Program, Further expansion of Adult Day Program
- Further analysis may consider pairing the co-morbidities experienced by patients with long lengths of stay, as well as how the number of excess bed days is affected by long-stay patients.
- MSAs across the North have received a summary of the project and its recommendations, along with site-specific data and information on how to launch an FE engagement project, with connections to Northern Health analytics.
- Other MSAs from across BC may wish to consider analysing ALC rates to determine its impact on patient access due to hospital overcapacity and contribute to building a greater understanding of the issue across BC.
- Dr Kane has provided a data tool for other sites and health authorities that wish to measure long stay impacts. (Download in the right column on this page.)