Annual Review Provincial Overview
Annual review activities
Seventy-one of the 76 eligible Medical Staff Associations (MSAs) have submitted their 2024/25 Annual Review (AR) report, see here for a copy of the full analysis included below.
- MSA and health authority-facilitated discussions on successes, challenges, and lessons learned over the last year.
- Highlighting key activities and results.
- Key priorities and planned activities for the upcoming year.
Section 1: MSA & HA facilitated discussions
- Engagement and collaboration among medical staff and health authority partners on shared priorities and physician-led initiatives highlight the significance of a team approach, open dialogue, and improved engagement. Enhanced collaboration fosters opportunities for feedback, influence and learning, ensures alignment, and improves engagement. Key priorities and initiatives include engaging on Recruitment and Retention efforts, inpatient care stabilization, facility needs, EHR implementation, and ED improvements. These efforts collectively contribute to a more engaged environment for physicians, ultimately benefitting patient care and operational effectiveness.
- Informal engagement spaces and events foster important connections and create a friendly atmosphere that enhances team building and helps retain physicians. Social gatherings, the physician lounge, and informal engagement events (e.g. recognition, engagement lunches) allow physicians and health authority leaders to interact, share ideas, build relationships, and promote a sense of community. Overall, these efforts strengthen teamwork and improve the medical staff experience.
- Health authority attendance at MSA meetings and establishing communication channels enhances coordination and clarity regarding on-site issues, leading to a better understanding of priorities, challenges, and information sharing. Meeting attendance creates opportunities for relationship building, transparent discussions, and timely problem-solving. Establishing communication channels addresses perceived disconnect and strengthens connections among medical teams and leadership.
- Regular and robust standing meeting formats enhance communication and encourage participation and relationships among medical staff. Key meetings, such as MSA meetings, working group meetings, and committees, foster a sense of community, trust, and collegiality while promoting active participation in MSA activities and projects. The emphasis on regular meeting structures highlights their role in fostering discussions, decision-making, and planning, ultimately leading to improved teamwork and a stronger connection among the medical staff.
- Foundational and strong local HA leader relationships are essential for successful collaboration and trust in the facility. Building solid partnerships between the MSA and local HA fosters open communication and effectively addresses the needs of medical staff. Accessible leadership creates a culture of respect and dialogue. Consistent leadership with strong connections to the physician community boosts engagement and collaboration, leading to better outcomes and a unified approach to engagement.
- Create more effective MSA meeting structures and offer flexible engagement opportunities to improve participation and alignment with MSA and HA meeting structures (e.g., LMAC), ensure team connection, and make participation more accessible and sustainable to reach a broader range of medical staff.
- Enhance communication and alignment by establishing clear communication channels for transparency, ensuring consistent follow-ups, and streamlining messages and requests so that regular updates and structured oversight maintain momentum and foster accountability.
- Implement a stronger project accountability framework to improve tracking systems for timelines and scope, clearer communication of expectations, defined roles for project leads, detailed reporting on projects, and processes to measure project success for better alignment and timely completion.
- Increase awareness and visibility of MSA supports and opportunities by showcasing local successes, improving outreach, and highlighting project and engagement wins to encourage broader participation from all departments and medical staff.
- Medical staff face limited capacity to engage due to burnout and time constraints, which impacts capacity to participate in meetings, take on leadership roles, and collaborate on initiatives, ultimately impacting participation in engagement efforts.
- Ongoing staffing shortages among medical staff are leading to high turnover, burnout, and challenges in recruitment and retention.
- Frequent leadership changes and role vacancies in HA create challenges in building effective relationships, maintaining trust, and implementing new initiatives, ultimately impacting stability and staff morale.
- Communication gaps in health care decision-making impacts trust among physicians, leads to frustration over limited opportunities for consultation, and results in unresolved issues and decisions that may not reflect the local context.
- Managing FE funding within annual allocation impacts the initiation of new projects and initiatives, increases challenges in engaging physicians amidst growing demands, and imposes limitations on operational resources.
Section 2: Highlights and results
MSAs are requested to provide a summary of impactful activities, opportunities, strategies, or successes they would like to highlight in the annual review report. A total of two hundred forty-one activities were highlighted from throughout the province. These highlights are examined under the following seven themes associated with Facility Engagement (FE) outcomes and those identified from the reports:
Expected FE outcomes:
- Improved engagement within the MSA.
- Improved engagement with the health authority.
- Strengthened MSA capacity and capabilities.
- Improved quality of patient care and work environment (direct and indirect).
Emerging from the data:
- Recruitment and retention.
- Community engagement.
- Interdisciplinary engagement.
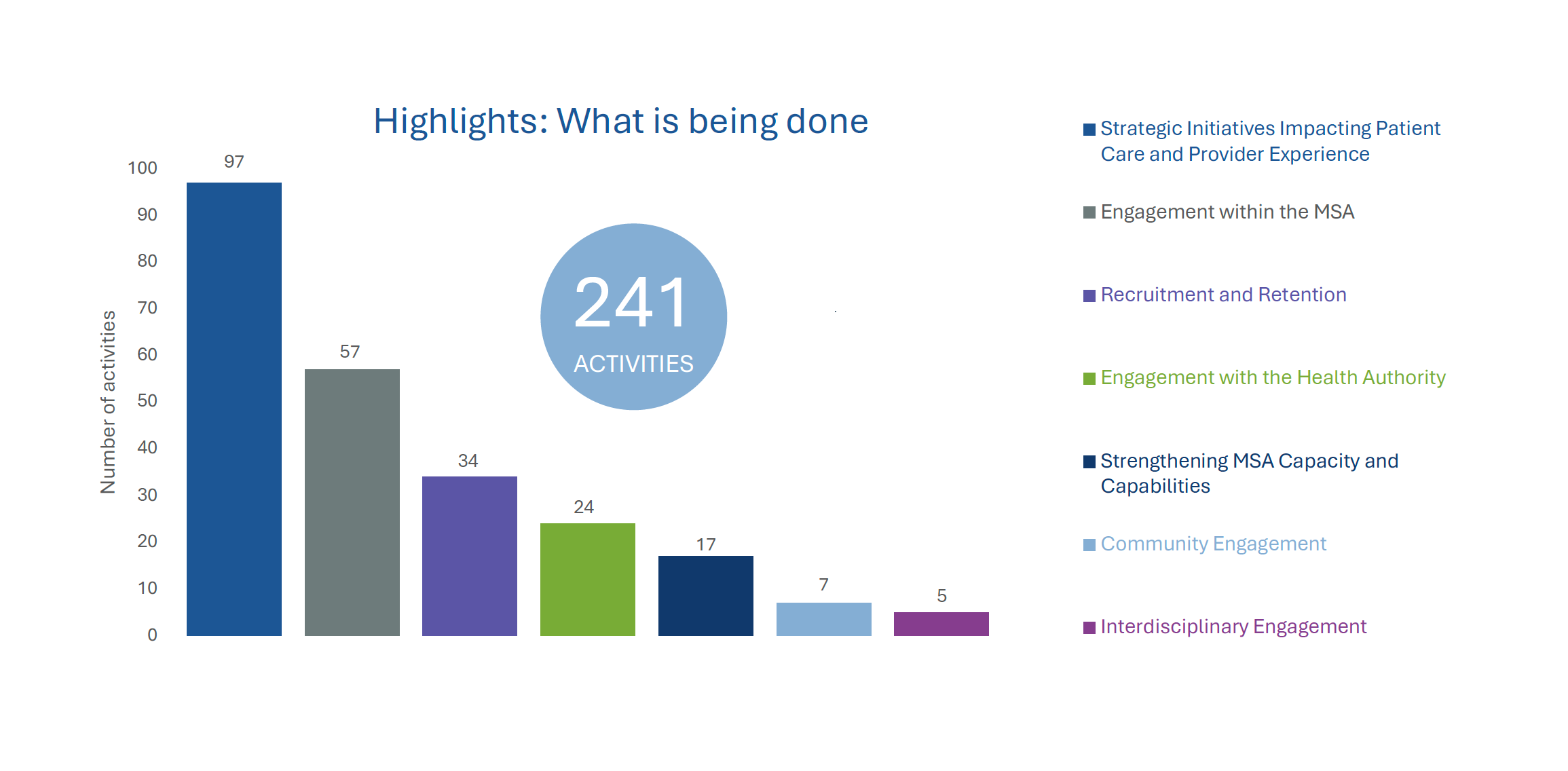
Strategic initiatives impacting patient care and physician experience
- Care optimization and flow.
- Clinical pathways, discharge, inpatient care stabilization, patient information and education.
- Quality Improvement.
- Physician Health and Wellness.
- Physician Wellness Committee and events, Local Peer Support Program, Commensality Group.
- Cultural Safety and Indigenous engagement professional development.
- SIMS training series, educational rounds, peer-to-peer training.
- EHR implementation and engagement.
- Civility Matters.
- Planetary health.
- Equity, diversity and inclusion.
- Supporting women in leadership.
Engagement within the MSA
- Effective MSA meetings for discussion, collaboration, and decision making.
- Communication platforms.
- Newsletters, websites, bulletins.
- Interdepartmental Collaboration Session.
- Physician recognition and appreciation.
- New physician welcomes, awards, Hello/Goodbye events, kudos.
- Formal engagement opportunities.
- Group professional development, team building, MSA events for focused discussion.
Recruitment and retention
- Marketing and advertising.
- Social media strategy, physician recruitment event.
- New physician onboarding.
- Buddy program, onboarding guide, welcome package, physician members on interview panels.
- Recruitment strategy.
- Survey spread, data project, R&R committees.
- Partnering with community on recruitment and retention.
- Retention Supports: Daycare spaces for health care workers.
- Recruitment incentives.
MSA and HA engagement
- Improving communication to enhance collaboration.
- Increased HA attendance at meetings, forums to support open communication.
- Physician involvement in priority areas.
- New hospital build.
- Collaborative decision making.
- Collaborative leadership models.
- Collaborative engagement.
- Collaborative engagement efforts for cross-site engagement, Healthcare Summit.
- Strengthened professional relationships.
- Monthly engagement lunches.
Strengthening MSA capacity and capabilities
- Governance enhancement.
- Transition from Society to FESC.
- Governance and operational optimization.
- HR best practices, governance and operational alignment.
- Succession planning and leadership sustainability.
- Strategic planning.
Community engagement
- Joint events with neighbouring physician groups.
- Partnering with community groups.
- Hospital Foundation.
- Regional MSA engagement.
- President's table.
Improved interdisciplinary engagement
- Interdisciplinary team meetings, improving team morale in the ER, appreciation.
Section 3: Key priorities for 2025/26
The top priorities MSAs identified for 2025/26 focused on the following themes:
- Improve communication and connection for medical staff engagement through effective meeting structures and strong communication to boost physician engagement.
- Enhance the medical staff experience by establishing a robust and cohesive community through team-building opportunities, physician wellness, professional development, recognition, socials, and welcoming spaces.
- Develop and support physician recruitment and retention activities via committees and projects designed to welcome new recruits and support an engaging work environment.
- Strengthen a unified physician voice by ensuring meaningful input and consultation, and leveraging venues to bring issues forward to influence decision-making on matters important to the medical staff.
- Support activities that positively impact patient care and patient/provider experience through system improvement, access to quality services, health equity, and optimal resources.
- Build strong, trusting relationships within the facility by collaborating with health authority leaders and partners.
Other top priorities include: physician health and wellness, partnership connection and relationship-building, cultural safety and Indigenous engagement, governance and leadership sustainability, and fostering collaboration on mutual priorities.